Currently, a large number of people suffer from osteochondrosis. Many of them do not even understand the existing problems. At the same time, if you do not start treatment on time, complications will occur, which will make you unforgettable. Osteochondrosis, like many other diseases, is "becoming young" and greatly deteriorates the quality of life, freeing people from their usual rhythms.
In our article, we will understand the disease itself and the medical methods of treatment.
Osteochondrosis and its types
Osteochondrosis is the deformation of articular cartilage, spinal bone tissue and intervertebral discs.
Osteochondrosis:

- waist (waist s-bone),
- Cervix,
- The chest.
Causes of osteochondrosis:
- Walk upright
- Spine curvature
- Spine injury,
- Flat feet,
- Frequently mentioned
- The position of the torso changes frequently,
- Staying in an uncomfortable position for a long time,
- Spinal overload,
- Lack of exercise and obesity,
- Malnutrition,
- Stress conditions.
Stages of development of osteochondrosis
- Due to some changes in the intervertebral discs, there will be vertebral instability. The spine is easily injured.
- The annulus fibrosis is broken. The nucleus pulposus of the intervertebral disc is herniated. Due to the formation of intervertebral hernias, spinal deformities are caused.
- Obvious pain syndrome occurs. Movement is restricted due to the formation of bone growth and ossification of spinal ligaments.
Symptoms of osteochondrosis
Waist (part
- Continuous aching back pain.
- Pain and numbness in the limbs.
- Reduced physical activity.
- Pain worsens when you exercise suddenly, lift weights, exercise, sneeze, and cough.
Cervical area
- Arm and shoulder pain, headache.
- Vertebral artery syndrome (burning headache, dizziness, head murmur, stains and "fly" in front of you).
Chest cavity area
- Pain in the internal organs, especially the chest ("piles" in the chest) and the heart area.
Confirm diagnosis
The diagnosis is appointed by the neurologist based on the patient's main complaint (pain syndrome, restricted mobility, etc. ). He examines the spine in the patient's standing, sitting and lying position (still and in motion). When examining the back, pay attention to the posture of the trunk, structural features, the lower corners of the shoulder blades, the side contours of the neck and waist, and the position of the shoulder straps. After that, doctors usually instruct patients to perform X-ray, computed tomography or MRI examinations, with the help of these examinations, the diagnosis can be clarified and specific, the degree of damage can be determined, and hidden deviations from the norm can be revealed. Based on the data obtained, the neurologist will prescribe an appropriate treatment plan. Usually, this is a complex therapy, including the use of drugs, massage, exercise therapy and other methods.
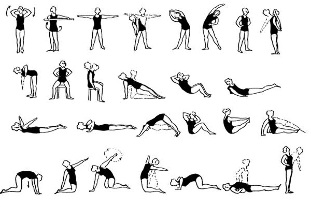
Therapeutic exercise for lumbar osteochondrosis
Medical treatment of osteochondrosis
First of all, it should be noted that in the initial stage of the development of osteochondrosis, in some cases, you can not use drugs. It is enough to use corrective gymnastics and various applicators to reduce the load and eliminate other diseases. If symptoms gradually increase and research shows that the characteristics change, drugs that help affect the cause and symptoms of osteochondrosis should be used.
During the deterioration of osteochondrosis, it is necessary to use drugs to treat osteoarthritis, the purpose is to relieve the inflammatory process, pain and metabolic process caused by internal intake or through injection of drugs.
As osteochondrosis is a systemic disease that negatively affects various organs and systems, comprehensive treatment should be given. The drugs used to treat osteochondrosis perform the following tasks:
- Painkiller
- Remove inflammation,
- Improve blood circulation in affected tissues,
- Cartilage repair,
- Restore the mobility of the joints,
- Eliminate depression caused by persistent pain.
So, what drugs can neurologists prescribe for osteochondrosis?
- NSAID (non-steroidal anti-inflammatory drugs).
Eliminate inflammation and pain. They can be used externally (gels, creams), internally (capsules, tablets) and in the form of injections (intramuscular, intravenous, subcutaneous).
- Vasodilators (vasodilators).
Due to muscle tension and pain in osteochondrosis, blood vessels narrow. In order to avoid adverse consequences in this context, doctors may prescribe vasodilators to achieve better repair effects.
- Muscle relaxants (muscle relaxants).
Muscle relaxants have relaxing and calming effects on muscles. Without these drugs, the healing process proceeds more slowly, because due to their properties, blood circulation is normalized, pain is reduced, mobility is restored, and affected tissues recover faster.
- Cartilage protector.
Cartilage protective agents will not be further damaged, they can stabilize the condition. Taking chondroprotective agents is long-term and lifelong, and this effect will not occur until at least 6 months after treatment. The chondroprotectant is used in internal, external and injection forms.
- Glucosamine
- Chondroitin
- Glucosamine + Chondroitin
- Glucosamine + Chondroitin + Vitamin
- tranquilizers (sedatives).
Long-term pain syndrome can cause stress and depression. In this case, valerian, motherwort, mixed herbal preparations should be prescribed. For more serious diseases, use antidepressants and use hypnotics to improve the process of falling asleep and sleep quality.
- Vitamins and vitamin-mineral complexes.
B vitamins are very important here because they can restore the sensitivity of the affected nerve fibers and relieve pain.
In order to fully enhance the body's functions, vitamin and mineral complexes can also be prescribed.

























